Understanding Hyperglycemia in Diabetes: Staying Hydrated for Optimal Management
Hyperglycemia, or high blood sugar, is a common complication of diabetes that can lead to serious health problems if left unmanaged. One often-overlooked aspect of managing hyperglycemia is hydration – drinking enough water plays a crucial role in maintaining healthy blood sugar levels.
The Science Behind Hydration and Blood Sugar
Drinking water helps regulate blood sugar levels by stimulating the pancreas to produce insulin, facilitating glucose uptake in cells, and reducing inflammation. Inadequate hydration can lead to increased blood glucose levels due to reduced insulin sensitivity. Research suggests that even mild dehydration can cause a 10-20% decrease in insulin sensitivity.
The Role of Hydration in Preventing Hyperglycemia
Proper hydration is essential for the body's natural processes, including glucose regulation. When we don't drink enough water, our bodies are unable to effectively transport nutrients and waste products – leading to fluctuations in blood sugar levels. Drinking at least eight glasses of water per day can help maintain healthy blood sugar ranges.
Debunking Common Myths About Hydration and Blood Sugar
One common myth is that consuming sugary drinks like soda or sports beverages will replenish fluids lost due to exercise. However, these drinks actually cause a significant spike in blood glucose levels – making it range of sugar level in blood even more challenging for people with diabetes to manage their condition.
Strategies for Staying Hydrated as You Age with Diabetes
As we age, our bodies undergo natural changes that affect hydration and blood sugar regulation. Older adults are at an increased risk of dehydration due to decreased thirst sensation, medications, or underlying medical conditions like kidney disease. Drinking water regularly throughout the day can 327 blood sugar level help mitigate these risks.
Monitoring Blood Sugar Levels for Optimal Hydration
To effectively manage hyperglycemia with hydration, it's essential to monitor blood sugar levels closely – especially in response to changes in fluid intake. Keeping a log of glucose readings and correlation with dehydration symptoms will provide valuable insights into your blood sugar monitoring log body's unique needs.
Maximizing the Benefits of Hydration for Diabetes Management
While staying hydrated is crucial, individual factors such as medication regimen, exercise level, or kidney function may influence how effective hydration is at regulating blood sugar levels. Consulting a healthcare provider to develop a personalized plan that incorporates optimal hydration and blood glucose monitoring can make all the difference in achieving healthy ranges.
Combining Hydration Strategies with Other Blood Sugar Management Techniques
By incorporating proper hydration practices alongside medication adherence, regular physical activity, and balanced eating habits – individuals with diabetes can significantly improve their ability to maintain healthy blood sugar levels. This holistic what does it mean when blood sugar is high approach allows for proactive management of hyperglycemia and reduces the risk of related complications.
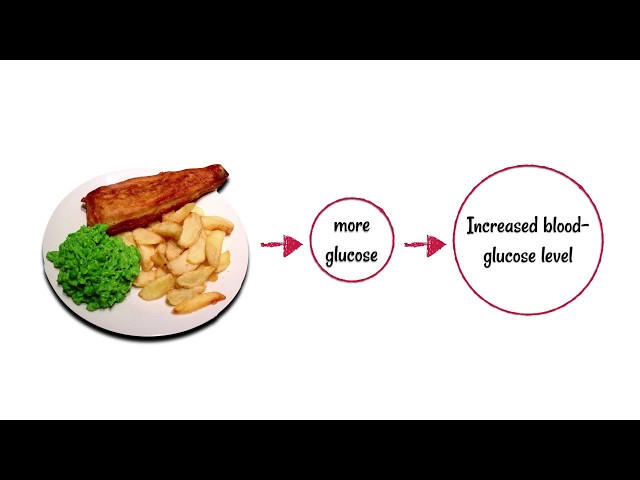
Biology video podcast: Subscribe to the podcast on iTunes: Twitter: Blood glucose levels must remain relatively constant. When glucose levels in the blood rise the pancreas secretes insulin, which tells the liver to convert glucose to glycogen and store it, thus returning glucose levels back to normal. When glucose levels fall, the pancreas recognises this change and secretes glucagon. Glucagon is a hormone that causes the liver to convert glycogen to glucose and release it, thus raising the blood glucose level back to normal. A person with diabetes doesn’t have an effective mechanism for blood glucose control. Type 1 diabetes is when the immune system attacks the cells in the pancreas that secrete insulin. Type 2 diabetes is when the bodies cells don’t respond correctly to insulin.